VQ Scan
What is a Nuclear Medicine VQ Scan? A ventilation–perfusion (VQ) scan is a nuclear medicine scan that uses radioactive material…
Read more
A paediatric hip ultrasound is an examination of a child’s hip joints with an ultrasound machine, which uses sound waves to form images or pictures of the hip joint. These sound waves cannot be heard by the human ear and cannot be felt by the child having the ultrasound.
Developmental dysplasia of the hip (DDH) is a condition where the ball and socket of the hip joint do not form normally.
In very young children, a hip ultrasound is used to see if the hip joints are forming normally or whether DDH is present.
A paediatric hip ultrasound is used when DDH is suspected or detected. DDH might be suspected to be present by your doctor or child health nurse when carrying out a clinical examination of your child. It might also be carried out if your child has a risk factor for DDH, such as being born breech or having a family history of DDH.
More than one paediatric hip ultrasound might be carried out over a period of a few months. This can be to show normal growth of the hip or to show if the abnormality is still present. If your child is having treatment for DDH, further hip ultrasounds might be carried out to show that the hip joint is in a good position (such as in a harness) and to show improvement in the appearance of the hip joint.
Paediatric hip ultrasound studies are also used to look for evidence of fluid in the hip joint. This can indicate joint inflammation, which might be associated with an infection.
There is no specific preparation for a paediatric hip ultrasound study. Your child will need to have their nappy and clothing removed to allow the ultrasound study to be carried out.
See the item ‘Making your child’s test or procedure less stressful – advice to help you and your family’.
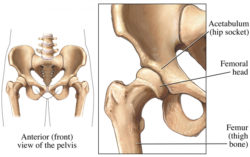
Figure 1
Your child will be placed on their side or back on an ultrasound bed, and their knees will usually be bent during the scan.
Clear gel is put on the area to be imaged, and a transducer (a small, smooth, handheld device) is placed on the hip joint and moved gently over the skin (see ultrasound). The gel allows close contact between the skin and the transducer, and allows the transducer to slide easily over the skin. Both hips will be examined during the study, which shows the ball (femur) and socket (acetabulum) parts of the hip joint.
The sound waves transmitted by the transducer produce an image of the hip joints on the ultrasound screen.
The ultrasound waves used for diagnostic ultrasound examinations cannot be felt by humans and do not cause any harm.
The gel used in the study washes off in water and should not mark or stain clothing. It might dry as a white powder on your child’s skin.
Your child will not feel any different before, during or after the test, and can return to school, kindergarten or child care after the study, unless there is a medical reason not to do so.
The time taken for the ultrasound varies with the age and level of cooperation of the child. It would usually take approximately 15–30 minutes, including time for the person carrying out the study to check that the quality of the images is satisfactory.
A paediatric hip ultrasound study is a safe procedure that causes no harm. The ultrasound examination might not show any abnormality, but sometimes the doctor can feel laxity (or looseness) of the joint, and when this is the case, further investigation might be required.
In older children, where the hip joints cannot be easily seen on ultrasound as the bones are too well developed, an X-ray of the pelvis might be required.
Ultrasound, with no potentially harmful X-rays, is ideally suited to children. The ultrasound examination can be carried out without the child having to be sedated or held completely still. Ultrasound studies have no side-effects.
A paediatric hip ultrasound can usually show the detail of the immature or abnormal hip joint very easily. Treatment of any abnormality can then be undertaken.
The images are usually obtained by a sonographer under the supervision of a radiologist (specialist doctor). The radiologist will interpret the images and provide a report to your doctor. It is not uncommon for the radiologist to also examine your child or watch some of the images being taken.
Ultrasound examinations are usually carried out in a private radiology practice or in a public or private hospital. Some doctors have their own ultrasound machine in their consulting rooms and might use it as a part of their examination of a patient.
The time that it takes your doctor to receive a written report on the test or procedure your child has had will vary, depending on:
Please feel free to ask the private practice, clinic or hospital where your child is having their test or procedure when your child’s doctor is likely to have the written report.
It is important that you discuss the results with the doctor who referred your child, either in person or on the telephone, so that they can explain what the results mean for you and your child.
If the ultrasound is carried out too early (before 5–6 weeks-of-age) or if the child has slightly delayed hip joint development, the ultrasound might appear abnormal, although the joint itself might develop normally without any treatment.
In most cases, DDH is detected soon after birth, but in some cases it is not noticeable until the child is walking. When detected early, the condition is easier to treat and treatment is usually effective. DDH is harder to treat when it is detected in older children. If left untreated, it might cause problems with the hip joint in later life, sometimes limiting mobility or causing pain.
American Academy of Orthopaedic surgeons – orthoinfo.aaos.org/topic.cfm?topic=a00347
Page last modified on 26/7/2017.
RANZCR® is not aware that any person intends to act or rely upon the opinions, advices or information contained in this publication or of the manner in which it might be possible to do so. It issues no invitation to any person to act or rely upon such opinions, advices or information or any of them and it accepts no responsibility for any of them.
RANZCR® intends by this statement to exclude liability for any such opinions, advices or information. The content of this publication is not intended as a substitute for medical advice. It is designed to support, not replace, the relationship that exists between a patient and his/her doctor. Some of the tests and procedures included in this publication may not be available at all radiology providers.
RANZCR® recommends that any specific questions regarding any procedure be discussed with a person's family doctor or medical specialist. Whilst every effort is made to ensure the accuracy of the information contained in this publication, RANZCR®, its Board, officers and employees assume no responsibility for its content, use, or interpretation. Each person should rely on their own inquires before making decisions that touch their own interests.